Implantable Cardioverter Defibrillators
Managing Cardiac Arrhythmias and Preventing Sudden Cardiac Death
In the context of LMNA-related cardiac conditions, the role of an ICD extends beyond just emergency intervention. It also provides continuous monitoring and data that can be used by healthcare providers to better understand a patient's cardiac health and refine treatment strategies. For patients with LMNA mutations, who may be susceptible to various cardiac complications, the use of an ICD can significantly enhance the quality of life and provide peace of mind, knowing that they have a constant guardian watching over their heart's rhythm.
S-ICD, T-ICD and EV-ICD
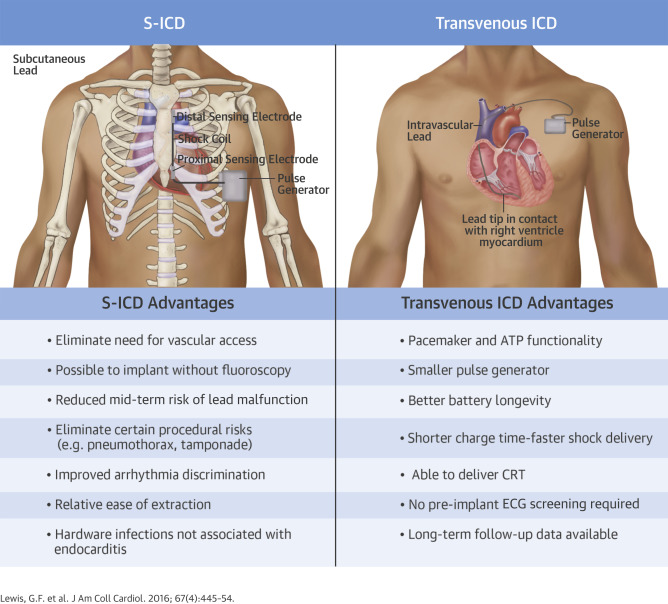
Historically there have been two commone types of ICDs, S-ICD (Subcutaneous Implantable Cardioverter-Defibrillator) and T-ICD (Transvenous Implantable Cardioverter-Defibrillator). Recently, Medtronic has launched the EV-ICD which is similar to the S-ICD and gains some of the benefits of the T-ICD.
S-ICDs are particularly suitable for individuals who have a high risk of sudden cardiac death due to ventricular tachyarrhythmias but do not require pacing or cardiac resynchronization therapy (CRT). S-ICDs are often chosen for younger patients, patients with limited venous access, or those at high risk for infections. S-ICDs do not have leads that enter the heart or vascular system. Instead, the electrode is placed just under the skin along the rib cage making it less invasive implantation procedure compared to T-ICDs with a lower risk of lead-related complications and vascular infections.
T-ICDs on the other hand, have leads that go through the venous system into the heart. In some cases, they are also capable of providing pacing therapy, defibrillation, and/or CRT making them a good choice for patients who require not only defibrillation capabilities but also pacing support. With the leads going through the venous system, they have a higher risk of lead-related issues and vascular infections. T-ICDs require a more invasive procedure for implantation.
EV-ICDs, are similar to S-ICDs in that there are no leads that enter into the heart. These ICDs can provide both pacing and defibrillation therapies. This ICD is also placed near the side of the patient similarly to the S-ICD.
The below image describes the primary differences between the S-ICD and T-ICD.
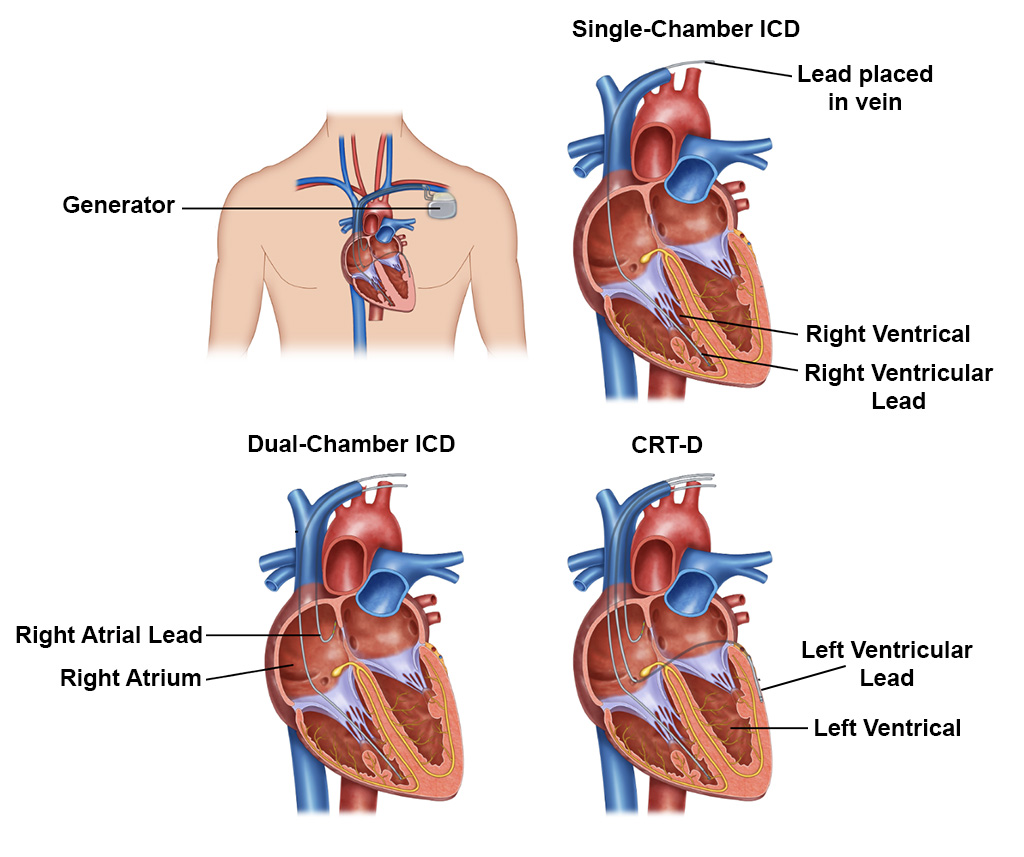
Types of T-ICDs
There are 3 main variants ICDs which are specific to transvenous systems (T-ICDs). The choice among these depends on the patient’s specific cardiac rhythm management needs, including pacing for bradycardia or synchronization in heart failure.
Single-Chamber ICDs have a single lead that is connected to one chamber of the heart, usually the right ventricle. It monitors the heart rhythm of the connected chamber. If it detects a dangerous tachyarrhythmia, it delivers a shock to restore normal rhythm. Single-chamber ICDs are typically used in patients who require only basic rhythm monitoring and intervention, predominantly in the ventricle.
Dual-Chamber ICDs have two leads that are connected to two chambers of the heart, the right atrium and the right ventricle. It monitors and can deliver therapy (pacing or defibrillation shocks) to both chambers. This allows for more sophisticated control of heart rhythms, as it can correct atrial and ventricular arrhythmias. Dual-chamber ICDs are often used in patients who have arrhythmias in both the atria and ventricles or who might benefit from the synchronization between the atrial and ventricular pacing, especially in cases of atrioventricular block or sinus node dysfunction.
Biventricular ICDs (Cardiac Resynchronization Therapy Defibrillator – CRT-D) have 3 leads that are connected to the right atrium, right ventricle, and additionally to the left ventricle (via a lead placed in the coronary sinus vein). Biventricular ICDs not only monitor and treat arrhythmias but also coordinate the contractions between the left and right ventricles (cardiac resynchronization). This can improve the efficiency of a weakened heart and is especially beneficial in patients with heart failure. They are specifically indicated for patients with systolic heart failure and a prolonged QRS duration on their ECG, which indicates dyssynchrony in the ventricular contractions. CRT-Ds are used to enhance cardiac function, reduce symptoms, and improve survival in selected patients with heart failure.
Post-Implantation Care and Lifestyle Considerations
Lifestyle adjustments are also an important aspect of living with an ICD. Patients are encouraged to gradually resume daily activities and engage in moderate exercise, avoiding activities that might impact the device site. Magnetic fields should be avoided, and care should be taken with the use of mobile phones and electronic devices. Travel is generally safe, but carrying an ICD identification card is advisable. Restrictions on driving may apply, especially for commercial drivers or those who have experienced loss of consciousness due to arrhythmias. Psychologically, adapting to an ICD can be challenging; support groups or counseling can be beneficial. Most patients with an ICD can return to their usual employment, though jobs involving physical labor or exposure to electromagnetic fields may require special consideration. Sexual activity can typically be resumed after recovery from the surgery, but any concerns should be discussed with a healthcare provider.
Overall, while living with an ICD involves certain considerations and adaptations, most patients can lead an active, fulfilling life. Regular medical follow-up, adherence to prescribed treatments, and mindful lifestyle choices are key to managing life with an ICD effectively.
Living with LMNA
Subscribe To Our Newsletter
Show Your Support
You can make a difference in various ways: by committing as a regular monthly donor, offering a single donation, organizing fundraising events both online and in person, contributing to our special tribute funds, or through your unique fundraising initiatives!